Tracheal Diseases
The trachea is a tube-shaped organ connecting the larynx and bronchi, composed of cartilage and membrane. In adults, its average length is 10–11 cm. The anterior part is cartilaginous, the posterior part is membranous, forming a horseshoe shape. It consists of 16–20 tracheal rings.
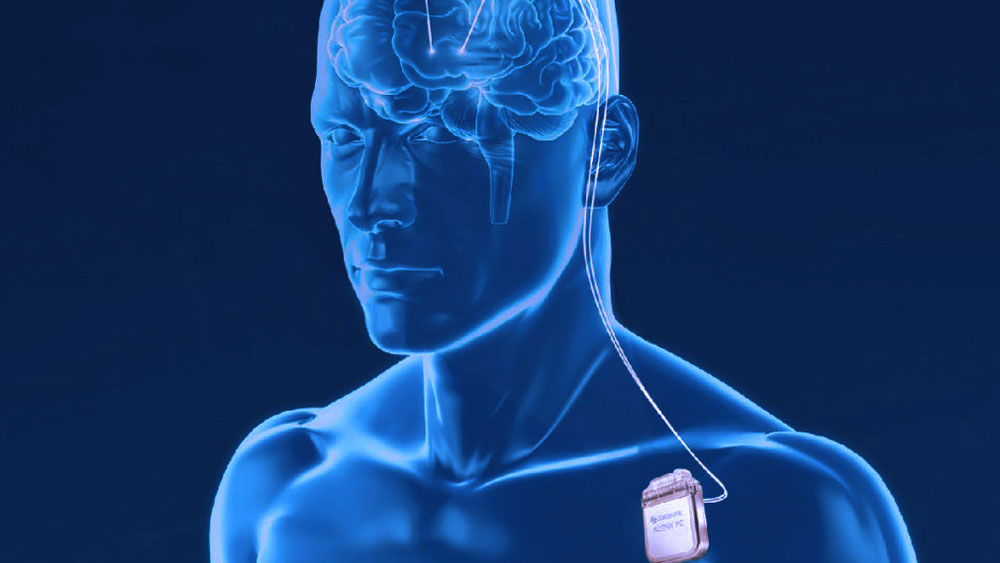
Trachea-Bronchial Stents
Airway stents are used in patients with recurrent tracheal narrowing or those not suitable for surgical reconstruction. They are most commonly applied for post-intubation stenosis.
Post-Intubation Stenosis
This is the most common benign cause of upper airway stenosis, especially seen after tracheostomy in intensive care patients. Symptoms usually appear 1–6 weeks after extubation. The most notable symptom is exertional shortness of breath, occurring when narrowing exceeds 50%. Other signs include stridor and changes in vocal function. Bronchoscopy and thoracic CT are the primary diagnostic tools.
Treatment depends on urgency:
-
Emergency: Oxygen and bronchodilators are given, and rapid bronchoscopy is performed.
-
Elective: Options include intermittent dilation, laser resection, and surgical resection. In benign tracheal stenosis, resection and anastomosis surgeries are highly successful.
Tracheal Tumors
Primary tracheal tumors are rare, with an incidence of 0.2 per 100,000 people. In adults, they are usually malignant, while in children they are mostly benign.
Benign Tracheal Tumors
-
90% of pediatric tracheal tumors are benign.
-
The most common type is papilloma, often multifocal and associated with human papillomavirus types 6 and 11.
-
They typically regress during the transition to adulthood.
-
If treatment is necessary, bronchoscopic ablation is performed.
Malignant Tracheal Tumors
-
90% of primary tracheal tumors are malignant.
-
Most common types include squamous cell carcinoma and adenoid cystic carcinoma.
-
Symptoms include shortness of breath, wheezing, stridor, cough, and hemoptysis.
-
Some patients may be misdiagnosed with asthma or chronic bronchitis.
-
Diagnosis is based on computed tomography and bronchoscopy.
-
Surgical treatment is the first-line option.