Spinal Tumors
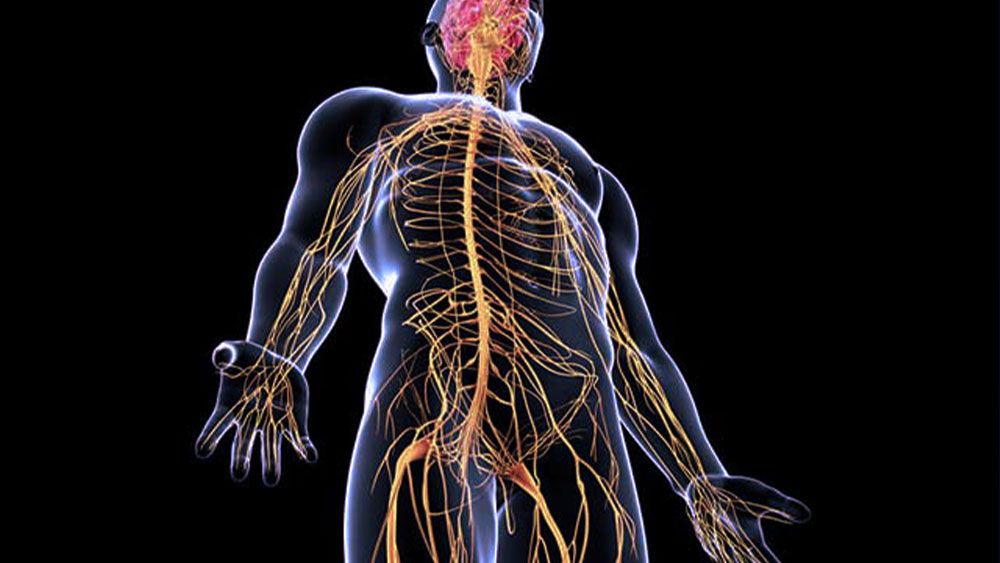
Spinal tumors are abnormal cellular growths that arise either in the vertebrae or in tissues surrounding the spinal cord. These tumors may originate in the spine itself (primary tumors) or may spread from another part of the body (metastatic tumors). Spinal tumors can compress the spinal cord and nerve roots, leading to pain, neurological deficits, and functional impairment. This article provides an overview of spinal tumors, the distinction between benign and malignant forms, surgical treatment options, and considerations during the recovery process.
General Overview of Spinal Tumors
Spinal tumors can develop in different regions of the spine and may affect both osseous and neural structures. They are classified as either primary or metastatic:
Primary Spinal Tumors: These originate directly within the vertebral bones or surrounding neural structures. Benign examples include osteoid osteoma and osteoblastoma, whereas chordoma represents a rare form of malignant primary spinal tumor.
Metastatic Spinal Tumors: These result from the spread of malignant cells from primary cancers located elsewhere in the body, such as the breast, prostate, or lungs. Metastatic tumors represent the most common malignant neoplasms of the spine.
Spinal tumors may cause significant symptoms including pain, sensory deficits, motor weakness, and reduced mobility, depending on their size, anatomical location, and effect on surrounding neural elements.
Differences Between Benign and Malignant Spinal Tumors
Spinal tumors may be benign (non-cancerous) or malignant (cancerous). Key differences between these two types include:
- Growth Rate: Benign tumors typically grow slowly and are less likely to invade surrounding tissues, whereas malignant tumors often grow rapidly and demonstrate local invasiveness.
- Metastatic Potential: Benign tumors do not metastasize, while malignant tumors possess the potential to spread to other parts of the body.
Treatment Complexity: Surgical resection is often sufficient for benign tumors, whereas malignant tumors may require adjunctive chemotherapy or radiotherapy.
- Threat to Life: Benign tumors are generally not life-threatening. Malignant tumors, however, can pose significant mortality risk due to their aggressive nature and potential for systemic dissemination.
Despite their classification, both benign and malignant spinal tumors may compress neural structures and therefore necessitate medical or surgical intervention.
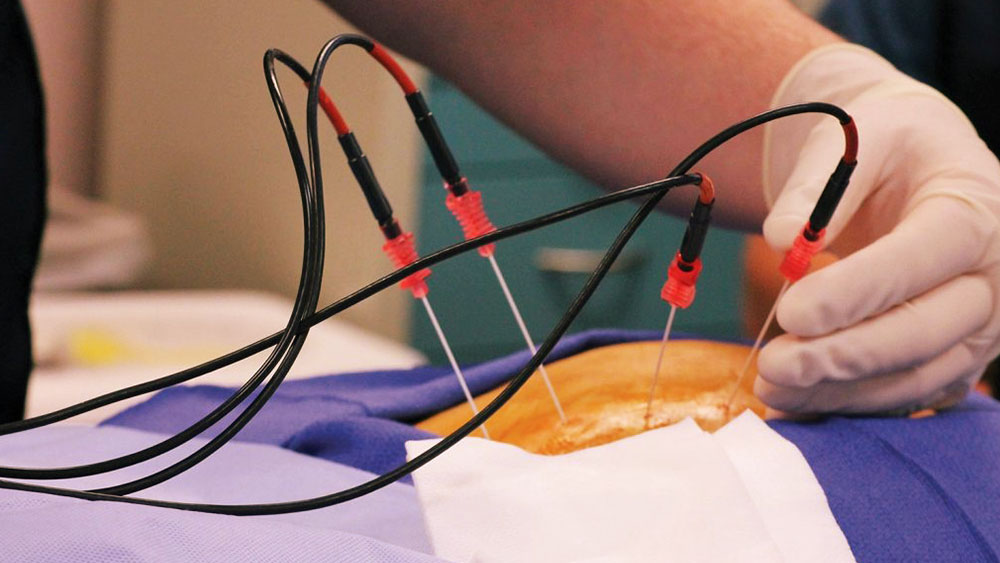
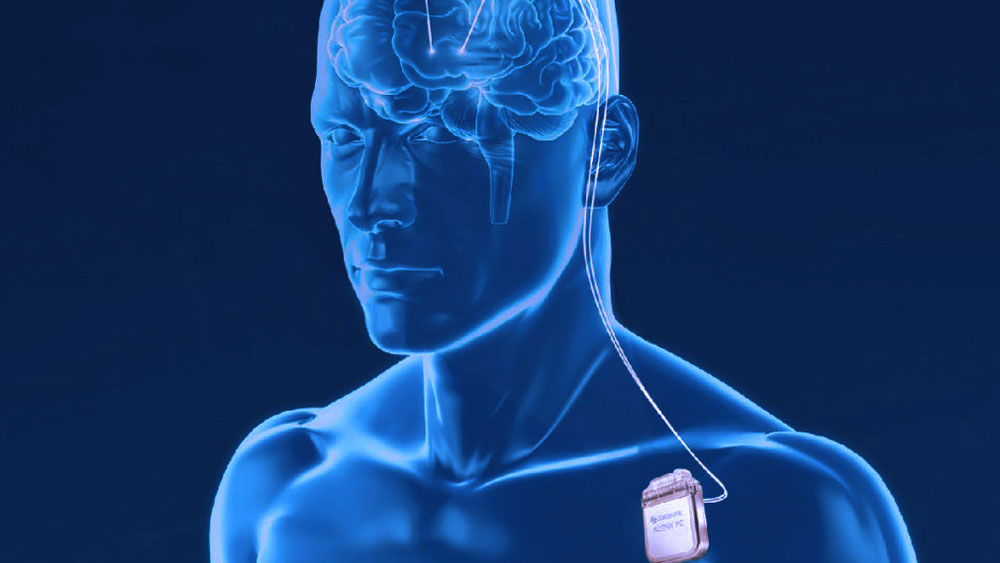
Surgical Treatment of Spinal Tumors
The surgical management of spinal tumors is guided by tumor type, size, location, and the patient’s overall health status. The primary objectives of spinal surgery are tumor resection and decompression of the spinal cord or nerve roots.
- Surgical Techniques: The complexity of tumor removal depends on the tumor’s location within the spine. In extensive lesions, en bloc resection (removal of the tumor along with surrounding tissue) is performed. Smaller tumors may be managed with partial resection.
- Spinal Stabilization: Large tumor resections may compromise spinal stability, necessitating the use of spinal fusion or metal implants to provide mechanical support and maintain alignment.
- Minimally Invasive Techniques: Advances in minimally invasive spine surgery reduce soft tissue damage, shorten recovery time, and lower the risk of postoperative complications.
Additional postoperative therapies may be required depending on the completeness of tumor resection and histopathological findings. In malignant tumors, adjuvant radiotherapy or chemotherapy is often administered to target residual cancer cells.
Quality of Life After Spinal Tumor Surgery
Surgical treatment for spinal tumors often results in improved quality of life due to pain relief and restoration of function. However, outcomes are influenced by the extent of surgery and the degree of pre-existing or intraoperative neurological damage.
Pain Reduction: Surgical decompression typically leads to significant alleviation of tumor-induced pain, resulting in enhanced physical comfort.
Functional Recovery: Patients with preoperative motor deficits, such as limb weakness or restricted range of motion, may regain partial or full function after surgery.
Psychological Benefits: Relief from tumor-related pressure and the resolution of cancer-related symptoms often contribute to improved emotional well-being and morale.
Postoperative Considerations and Patient Guidance
Recovery after spinal surgery varies based on the scope of the procedure and the patient’s condition. Several factors are critical for optimizing outcomes:
Physical Activity and Rehabilitation: Adherence to a structured physiotherapy program strengthens spinal support muscles and promotes functional recovery while maintaining spinal stability.
Weight Management: Excess body weight increases mechanical stress on the spine. Maintaining a healthy weight supports long-term spinal health.
Balanced Nutrition: A diet rich in bone-supportive vitamins and minerals facilitates tissue healing and structural recovery.
Regular Follow-up: Particularly in cases of malignant tumors, routine follow-up is essential to detect recurrence at an early stage.
By adhering to medical recommendations and implementing necessary lifestyle adjustments, patients who undergo spinal surgery can achieve substantial improvements in quality of life. Patient compliance plays a pivotal role in preserving spinal integrity and ensuring long-term recovery.