ENDOSCOPIC (FULLY CLOSED) DISCECTOMY
For many individuals struggling with cervical or lumbar, endoscopic (fully closed) lumbar disc surgery offers a source of hope. On this page, we explain what endoscopic disc surgery is, how it works, and how it may be a solution for you.
What Is Endoscopic Disc Surgery?
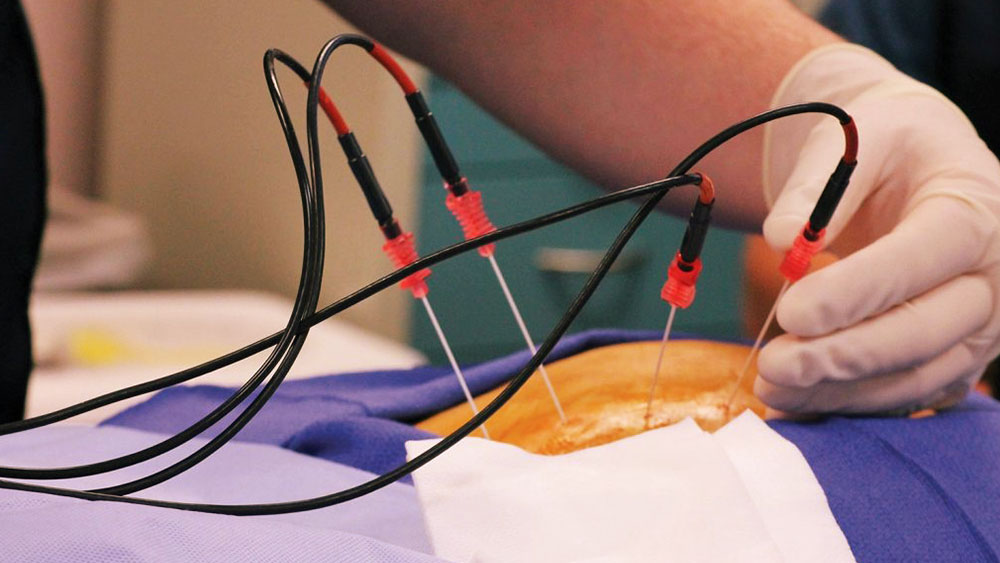
Endoscopic disc surgery is a minimally invasive surgical technique used to treat herniated discs in the spine. Through a small 7 mm incision—roughly the size of a pencil tip—a herniated disc fragment is removed with the aid of a camera. Compared to traditional surgery, this approach involves smaller incisions and less muscle disruption, offering significantly faster recovery times. Thanks to endoscopic disc surgery, many patients have experienced relief from back pain and a substantial improvement in their quality of life.
Before and After Surgery
Before surgery, your doctor will conduct a thorough evaluation and determine the most appropriate treatment plan for you. You will also receive instructions on how to prepare for the procedure.
After surgery, your recovery will be supported with rest and possibly physical therapy. It is crucial to follow your doctor’s post-operative recommendations closely during this period.
Frequently Asked Questions
- What are the risks of this surgery?
As with any surgical procedure, endoscopic lumbar discectomy carries certain risks. These may include dural tears (injury to the spinal cord lining), intraoperative bleeding, wound infections, or recurrence of the herniation—similar to complications seen in other spinal surgeries.
- How soon can I return to normal activities after the operation?
Patients are typically mobilized 2–3 hours after the procedure. Depending on the individual case, they may return home the same evening or be discharged the following morning.
- Am I a suitable candidate for endoscopic disc surgery?
In general, most types of disc herniation can be treated with endoscopy. However, the final decision depends on MRI results and your doctor’s clinical examination.
- What kind of rehabilitation program should I follow after surgery?
If there was no significant muscle weakness before surgery, physical therapy is usually not required. Beginning in the third week post-op, patients may start light exercises such as swimming and low-intensity walking to strengthen the lumbar muscles.
Final Thoughts
Endoscopic disc surgery can be a highly effective treatment option for individuals suffering from cervical and lumbar disc hernia. To determine the best solution for your condition, feel free to ask our specialists