Deep Brain Stimulation (DBS) Surgery
Deep Brain Stimulation (DBS) is a modern and effective surgical technique used in the treatment of various neurological diseases. By modulating specific brain regions through electrical stimulation, DBS plays a significant role in managing movement disorders and certain psychiatric conditions. This article provides detailed information about what DBS is, how it is performed, and which conditions it is used to treat.
What is Deep Brain Stimulation?
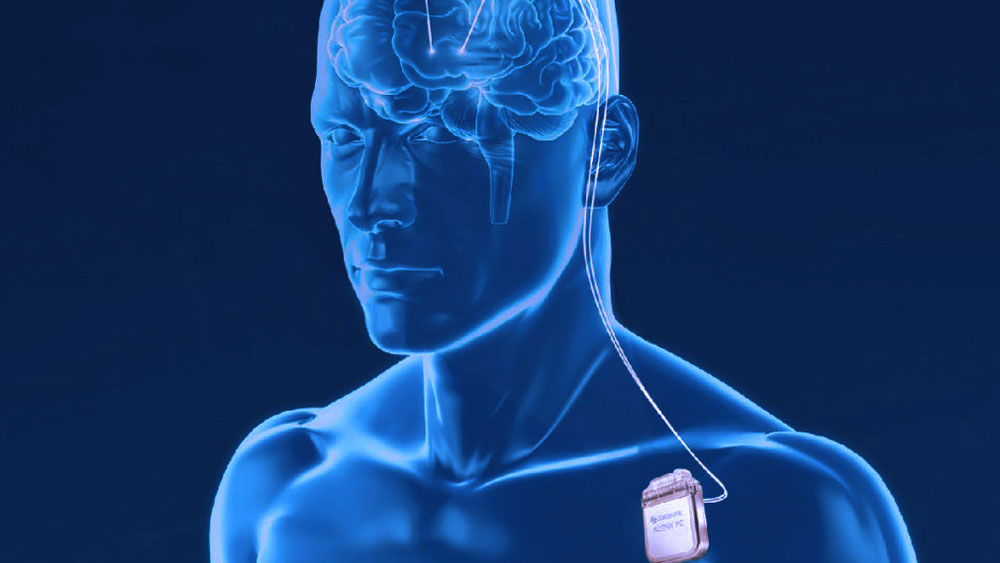
DBS is a treatment method involving the placement of fine electrodes into specific target areas deep within the brain. These electrodes deliver continuous or controlled electrical impulses to regulate abnormal neural activity, aiming to alleviate symptoms without permanently altering brain structures.
DBS is a reversible procedure—devices can be turned off, adjusted, or completely removed—making it a more flexible option compared to permanent surgical interventions.
Conditions Treated with DBS
DBS is primarily used to treat the following conditions:
a) Parkinson’s Disease
DBS helps alleviate motor symptoms such as tremors, stiffness, and slowness of movement. It is especially effective in patients who no longer benefit from medications or experience significant side effects.
b) Essential Tremor
As the first condition for which DBS was approved, it helps control involuntary tremors in the hands, head, or other parts of the body.
c) Dystonia
DBS can improve quality of life by controlling involuntary muscle contractions and spasms.
d) Obsessive-Compulsive Disorder (OCD)
In severe and treatment-resistant OCD cases, DBS can target brain areas involved in emotion and thought regulation.
e) Epilepsy
For patients with drug-resistant epilepsy, DBS can reduce the frequency and severity of seizures.
f) Tourette Syndrome
DBS helps reduce tics by modulating dysfunctional neural circuits in the brain.
The DBS Procedure
1) Patient Evaluation
A comprehensive neurological and psychiatric evaluation is performed. MRI and CT scans help identify the exact target areas, and a multidisciplinary team conducts electrophysiological tests.
2) Surgical Preparation
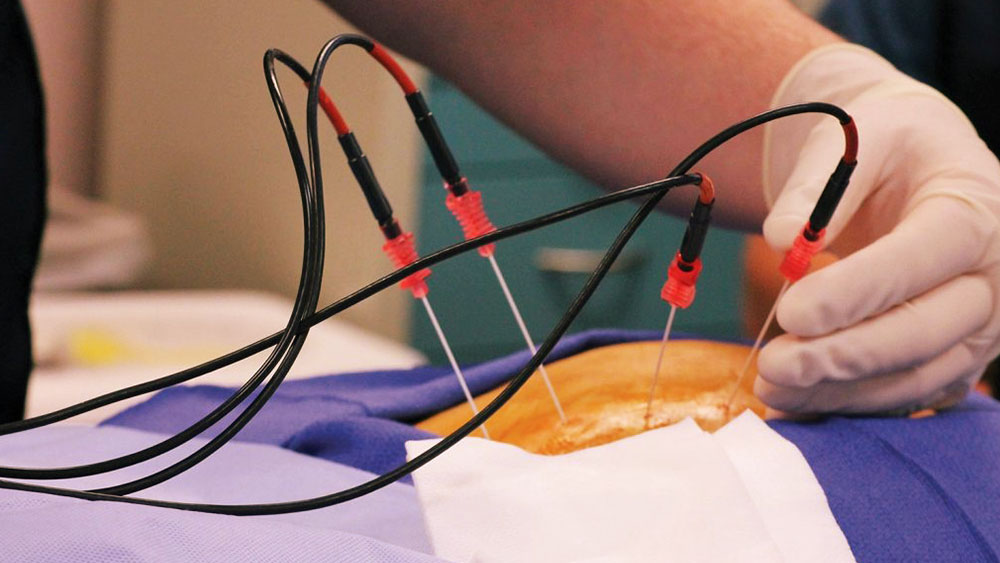
DBS can be done under local and general anesthesia, allowing real-time assessment of brain function. The patient’s head is stabilized using a stereotactic frame, ensuring accurate electrode placement.
3) Electrode Placement
Fine electrodes are inserted into the target brain regions. During surgery, neurophysiological monitoring and real-time symptom relief help confirm accurate placement.
4) Battery Implantation
The electrodes are connected to a pulse generator implanted under the skin in the chest. This battery-powered device provides the electrical stimulation and is externally programmable.
5) Programming and Adjustment
After surgery, the device is programmed and calibrated to the patient’s specific needs. Parameters are adjusted regularly to maximize symptom control and minimize side effects.
Advantages of DBS
Symptom Relief: Significantly reduces tremors, rigidity, and tics.
Reversible and Adjustable: The device can be turned off, reprogrammed, or removed.
Reduced Medication Use: Often lowers the required dose of medications in diseases like Parkinson’s.
Long-Term Effectiveness: With proper care and follow-up, DBS can remain effective for many years.
Potential Risks and Side Effects
Although generally safe, DBS surgery involves some risks:
Bleeding and Infection: Rare but possible during brain surgery.
Electrode Misplacement: Incorrect positioning can reduce effectiveness.
Stimulation Side Effects: May include tingling, speech issues, or balance problems.
Device Malfunction: Battery depletion or technical issues can occur but are uncommon.
Who is a Good Candidate?
DBS is not suitable for every patient. Ideal candidates typically include those who:
Have medication-resistant symptoms,
Suffer from significantly impaired quality of life due to motor disorders,
Are in generally good health and can undergo surgery.
Thorough preoperative assessment is essential for determining eligibility